What Are SOAP Notes?
SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan. The framework provides a structured approach to clinical documentation ensuring that all relevant information is captured and communicated effectively.
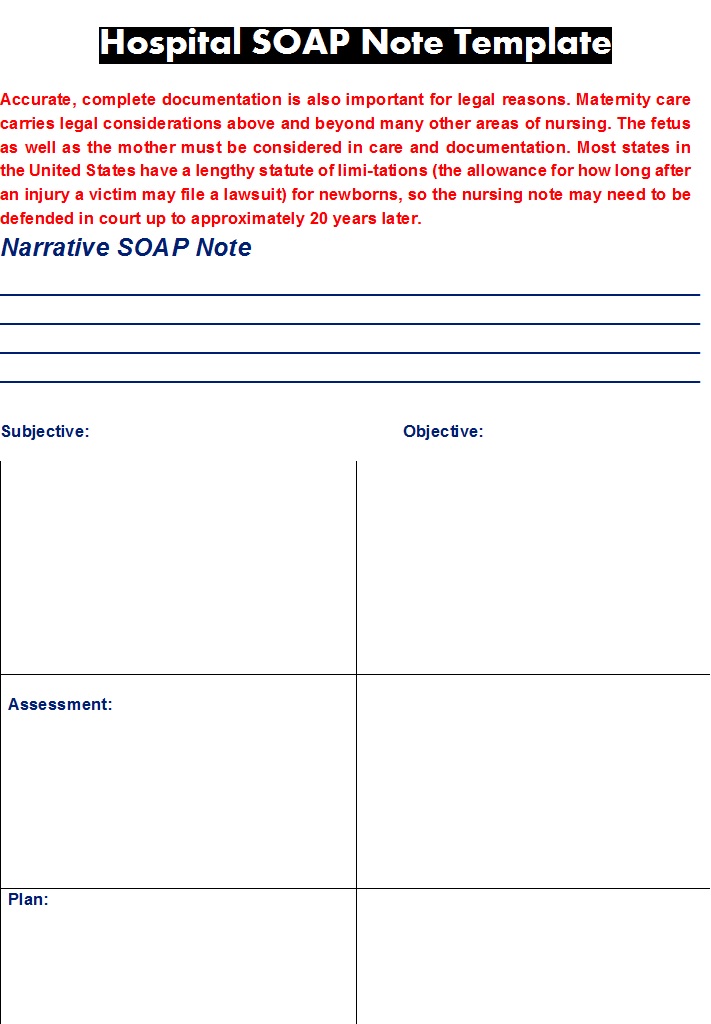
For a Hospital, it is very important to stay on top of every thing. It ensure continuity of care, facilitates communication among healthcare providers, and supports accurate billing and reimbursement with the help of organized daily reports. One widely used method for organizing clinical documentation ia the SOAP notes Templates.
Benefits Of Making SOAP Notes:
- SOAP notes facilitates clear and concise communication among healthcare providers, reducing errors and misinterpretations.
- provides a comprehensive overview of a patient’s condition, SOAP notes templates support informed decision-making and continuity of care.
- It streamlines clinical documentation, reducing the time spent of charting and focus more on patient care.
- ensure compliance with regulatory requirements and accreditation standards, reducing the risk of audits and penalties.
SOAP Notes Templates In Word:
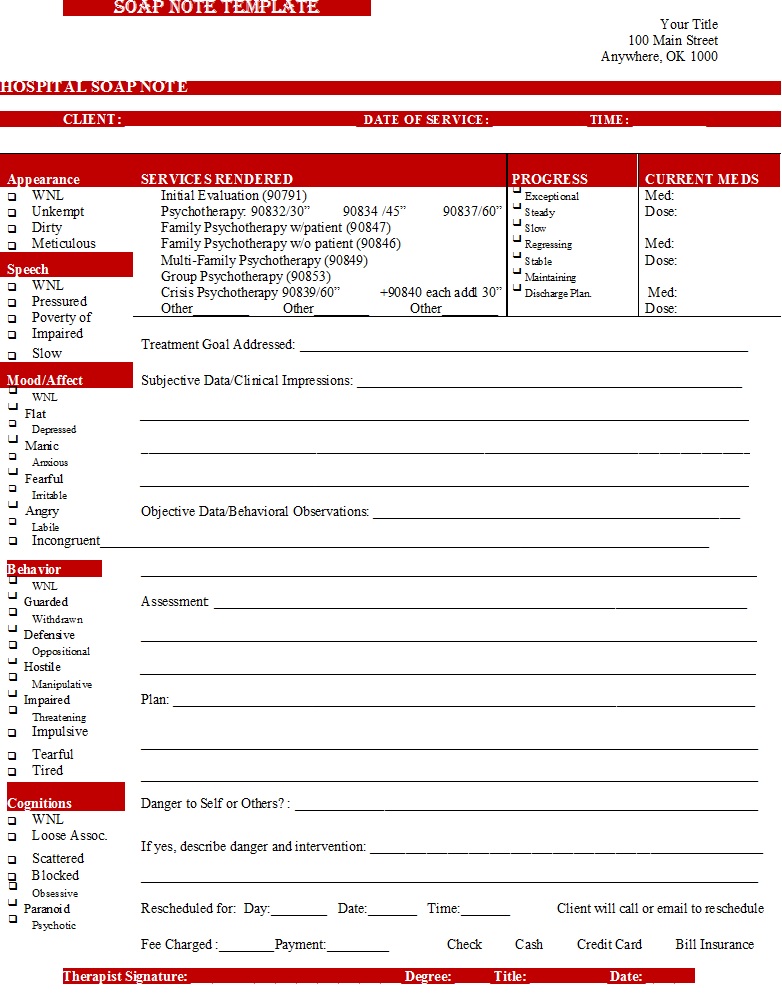
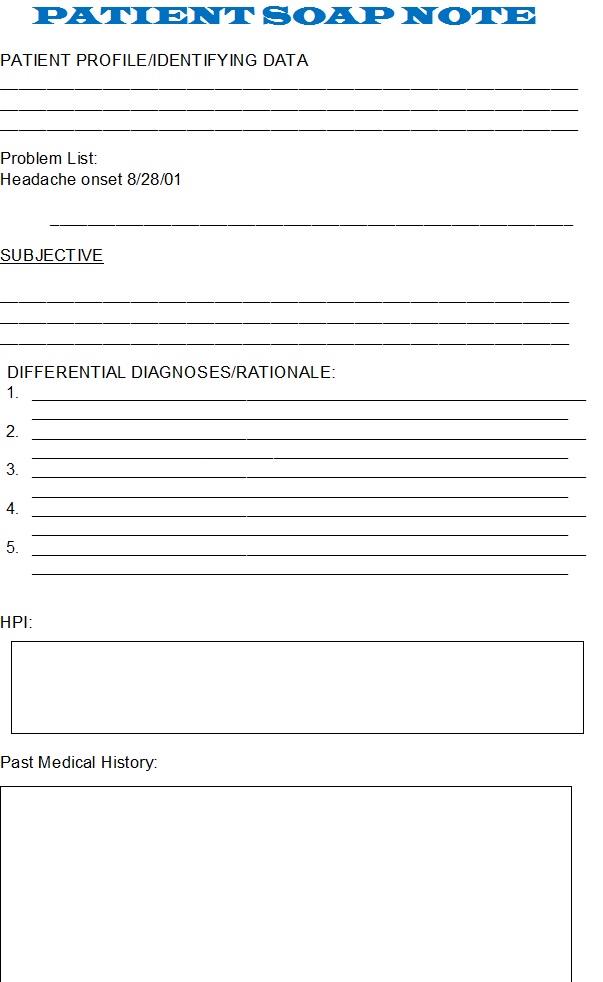
Patient SOAP Note Templates:
How To Make A SOAP Note?
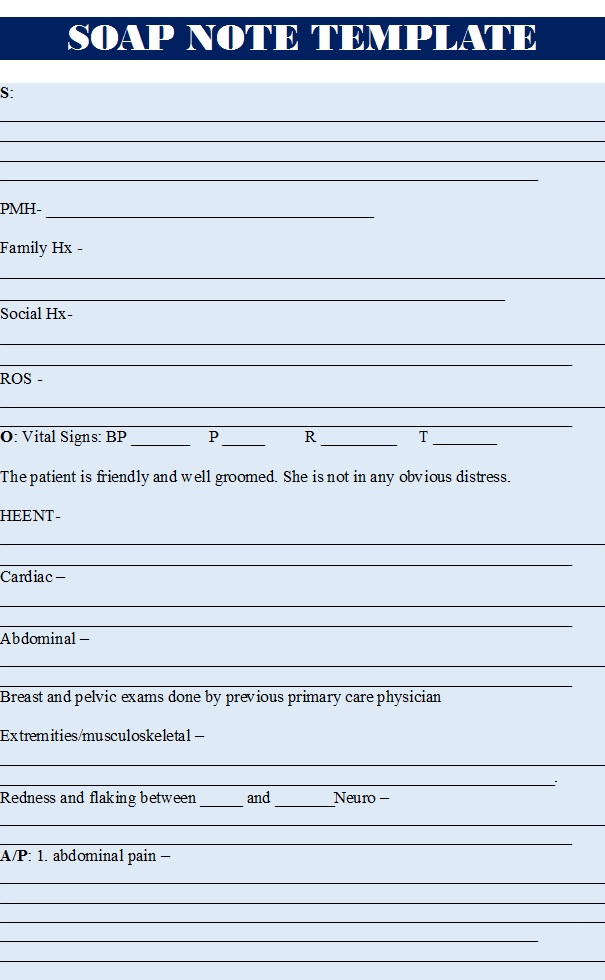
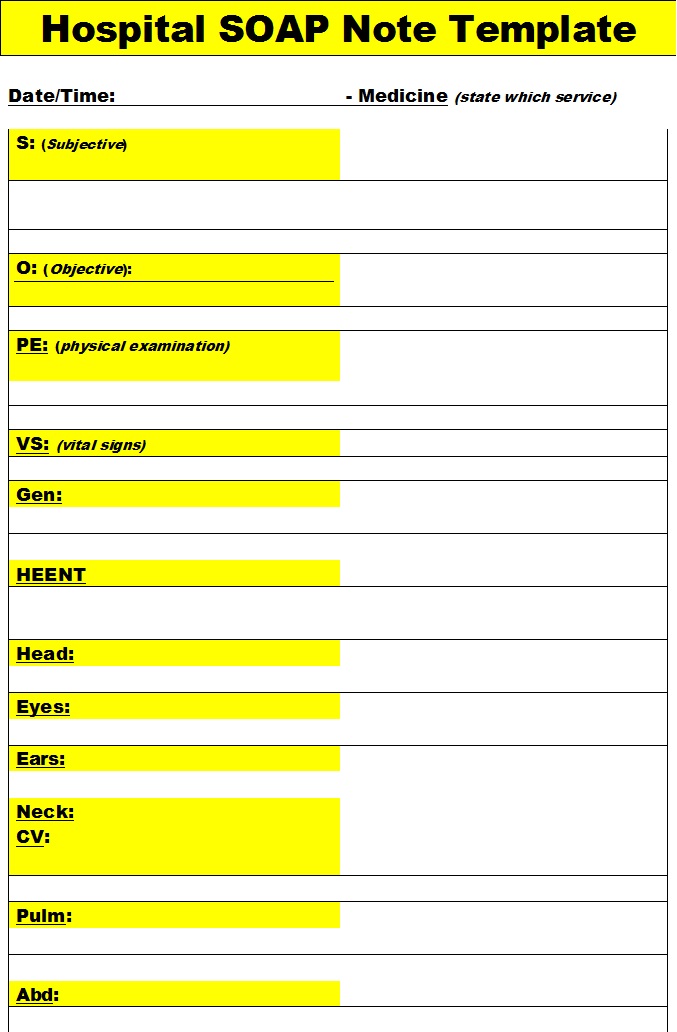
A comprehensive SOAP note template should include the following components:
- Subjective: Patient’s subjective experience, including chief complaint, history of present illness, and review of system.
- Objective: finding including vital signs, physical examination results, laboratory and diagnostic test results and other relevant data.
- Assessment: Healthcare provider’s assessment of the patient’s condition diagnosis and relevant medical history.
- Plan: It plan for patient’s treatment, medication, referrals, and follow-up appointment.
Medical SOAP Note Samples:
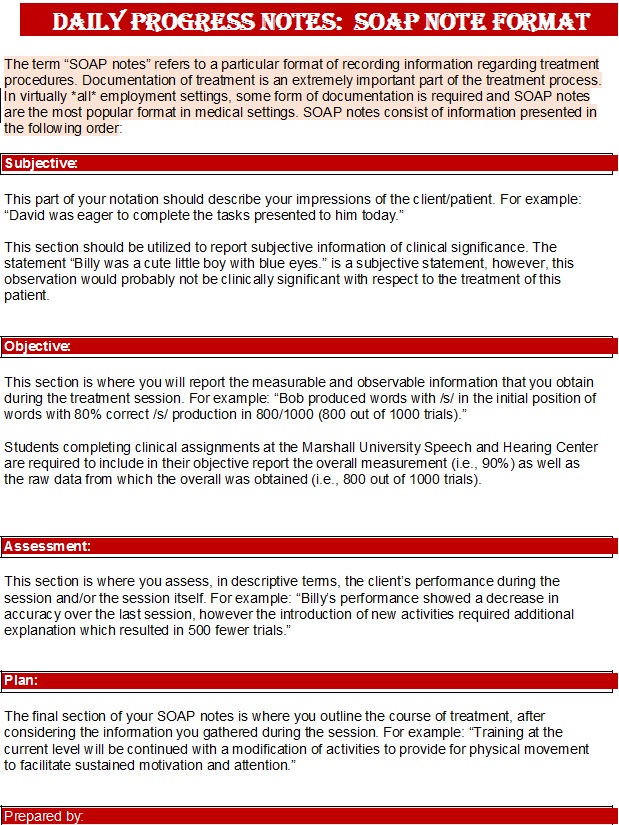
Patient Progress Notes Templates:
Progress Notes includes update on patient’s subjective experience, including pain, symptoms and concerns. Same goes with the objective findings. It also update assessment, including diagnosis, differential diagnosis and relevant medical history. And finally puts emphasis on treatment plan, any changes, referrals, follow-up appointments etc.